A diet high in saturated fats is just asking for problems.
Old way of thinking, based on flawed studies dependent on food questionnaires, corruption, and fraud.
SFA = saturated fatty acid
CVD = cardiovascular disease
CHD = coronary heart disease
Journal of the American Heart AssociationDietary Fatty Acids, Macronutrient Substitutions, Food Sources and Incidence of Coronary Heart DiseaseThis observational study found no strong associations of total fatty acids, SFAs, monounsaturated fatty acids, and polyunsaturated fatty acids, with incident CHD.
By contrast, we found associations of SFAs with CHD in opposite directions dependent on the food source.
https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019814Journal of the American College of CardiologySaturated Fats and Health: A Reassessment and Proposal for Food-Based RecommendationsThe dietary recommendation to reduce intake of SFAs without considering specific fatty acids and food sources is not aligned with the current evidence base. As such, it may distract from other more effective food-based recommendations, and may also cause a reduction in the
intake of nutrient-dense foods (e.g., dairy, unprocessed meat) that may help decrease not only the risk of CVD, type 2 diabetes, and other noncommunicable diseases, but also malnutrition, deficiency diseases, and frailty, particularly among “at-risk” groups.
https://www.jacc.org/doi/10.1016/j.jacc.2020.05.077U.S. National Institutes of Health's National Library of MedicineDietary Saturated Fats and Health: Are the U.S. Guidelines Evidence-Based?Multiple reviews of the evidence have demonstrated that a recommendation to limit consumption of saturated fats to no more than 10% of total calories is not supported by rigorous scientific studies. Importantly, neither this guideline, nor that for replacing saturated fats with polyunsaturated fats, considers the central issue of the health effects of differing food sources of these fats. The 2020 DGAC review that recommends continuing these recommendations has, in our view, not met the standard of “the preponderance of the evidence” for this decision.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8541481/The British Medical JournalAssociation of carbohydrate and saturated fat intake with cardiovascular disease and mortality in Australian women[/b]
In middle-aged Australian women, moderate carbohydrate intake (41.0%–44.3% of TEI) was associated with the lowest risk of CVD, without an effect on total mortality.
Increasing saturated fat intake was not associated with CVD or mortality and instead correlated with lower rates of diabetes, hypertension and obesity.https://heart.bmj.com/content/108/12/932CR = carbohydrate restricted diet
LF = low fat diet
U.S. National Institutes of Health's National Library of MedicineLow carbohydrate diets improve atherogenic dyslipidemia even in the absence of weight lossA recent report of Krauss et al. (AJCN, 2006) separates the effects of weight loss and carbohydrate restriction. They clearly confirm that
carbohydrate restriction leads to an improvement in atherogenic lipid states in the absence of weight loss or in the presence of higher saturated fat. In distinction, low fat diets seem to require weight loss for effective improvement in atherogenic dyslipidemia.
Compared to weight loss on a LF diet,
the high saturated fat CR diet with no weight loss resulted in better improvements in LDL peak size, TAG, HDL, and the ratios total cholesterol/HDL and apoB/ApoA-1, that is, the effects are not equivalent; CR is significantly better than weight loss in the presence of LF for atherogenic dyslipidemia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1488852/The American Journal of Clinical NutritionEffects of a low-carbohydrate diet on insulin-resistant dyslipoproteinemia—a randomized controlled feeding trialA low-carbohydrate diet,
high in saturated fat, improved insulin-resistant dyslipoproteinemia and lipoprotein(a), without adverse effect on LDL cholesterol. Carbohydrate restriction might lower CVD risk independently of body weight
https://ajcn.nutrition.org/article/S0002-9165(22)00119-8/fulltextU.S. National Institutes of Health's National Library of MedicineSeparate effects of reduced carbohydrate intake and weight loss on atherogenic dyslipidemiaWith the 26%-carbohydrate diet,
lipoprotein changes with the higher saturated fat intakes were not significantly different from those with the lower saturated fat intakes, except for LDL cholesterol, which decreased less with the higher saturated fat intake because of an increase in mass of large LDL.
https://pubmed.ncbi.nlm.nih.gov/16685042/Fat is the most calorie dense food there is.
And that is a very good thing, because it easily gets you to your daily caloric and nutritional needs with far less food volume. Fat, especially animal saturated fat, is far more satiating than carbs, making it more difficult to overconsume.
Unlike carbs, fat is also essential as it contains highly bioavailable essential fatty acids, fat soluble vitamins, and dietary cholesterol, all necessary for optimal health.
KD = Ketogenic Diet
Manipulation of Dietary Intake on Changes in Circulating Testosterone ConcentrationsFor the hormonal system to function optimally, fat becomes an important macronutrient as it’s the backbone for steroid hormone production [81].
Cholesterol, a dietary fat component, is one of the building blocks for testosterone production [81]. Considering that high-fat diets (HFD) increase cholesterol levels, increases in dietary fat consumption have been suggested to potentially result in an increase in testosterone production [85].
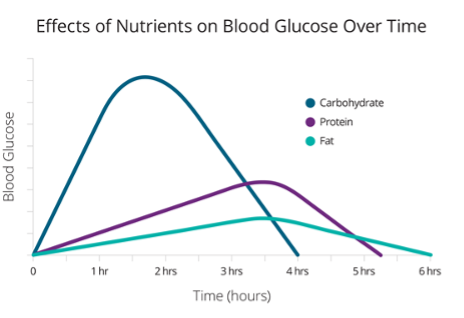
It has been suggested that increases in testosterone concentrations resulting from a KD are related to the high dietary intake of cholesterol [88].https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8538516/And of the three macronutrients, fat has the lowest impact on blood glucose and insulin levels.